Frequently Asked Questions
Questions? We’re here to help.

How can I change my Primary Care Provider (PCP)?
Under Quick Links, click “Change Your PCP” or, under My Health Plans, click “Change PCP.” If you know the name or practice of the doctor you’d like to choose, type it in. You can search for a new PCP in your area by selecting from the drop down and typing the city, county or zip code in the field to the right. You can also search by the hospital the physician is affiliated with, by the sex of the doctor or by the language the physician speaks. Once you press Submit, browse through the list of doctors and press Select when you find the physician you would like. This request will go directly to your Customer Service department who will process the request. Approved change requests will take effect on the date the request is submitted. If there is a change to your member information, such as a change in your PCP, you will be mailed a new ID card within 7 to 10 days.
What is a vaccine or immunization?
A vaccine is a type of medicine that is usually given to you as a shot with a needle. The medicine in the shot protects your body from one or more diseases. When you get this medicine, your body learns how to fight the disease so that you will not get sick from it. This is called “immunization.”
Are vaccines safe?
Yes. Vaccines are very safe. If any side effects occur from vaccinations, they are very minor, such as soreness where you received the shot, fussiness; or a low-grade fever. Serious side effects, like allergic reactions, are very rare, and doctors are trained to treat them.
Why do we get the same shot more than once?
Some vaccines take more than one dose to give you full protection. Other vaccines stop working after a while, so you need to get them again. Make sure that you get every dose of all of your vaccines. This is the only way to make sure that you are protected from the disease.
What is a D-SNP plan?
D-SNP stands for Dual Eligible Special Needs Plan. These plans enroll individuals who are entitled to both Medicare and Medicaid. These plans must cover the same Medicare services that all Medicare Advantage plans cover and may also cover extra services. To join a D-SNP plan you must meet the eligibility requirements. To find out more about Johns Hopkins Advantage MD D-SNP (HMO) see your:
To see if you qualify for Medicaid visit www.marylandhealthconnection.gov.
What is the Advantage MD Flex Card?
Advantage MD’s Flex Card is a prepaid card to help eligible members pay for monthly healthy food and utility expenses. Members receive a Benefits Mastercard® Prepaid Card. Advantage MD loads the card every month with $90 ($45 for groceries and $45 for utilities).
How do I qualify for a Flex Card?
Members must meet criteria based on eligible health conditions. Members must complete a consult visit with their provider, and the provider must submit a claim to Advantage MD. The claim must contain one or more diagnosis codes that correspond to a qualifying condition (qualifying conditions are noted in your Evidence of Coverage).
How much money is on the Flex Card from Advantage MD?
The Flex Card is loaded with $90 every month ($45 for healthy food and $45 for utilities).
Can I get a Flex Card?
The Advantage MD Flex Card is included at no extra cost for eligible members* in the D-SNP (HMO) plan. Not all members will qualify, but if you meet the chronically ill eligibility requirements, Advantage MD will send you a Flex Card after you enroll.
What expenses can I pay for with my Flex Card?
You can see what is eligible for purchase by visiting JHHP.NationsBenefits.com or through the Benefits Pro™ App.
Please keep in mind:
- Product availability and price may vary by retailer.
- This card is not a credit card or a gift card.
- You cannot use this card to obtain cash.
How do I activate my Flex Card?
You have two convenient ways to activate your card:
- Log in to your personalized Benefits Pro™ Portal at JHHP.NationsBenefits.com/Activate
- Call 877-205-8005 (TTY: 711)
How do I use my Flex Card for expenses?
You can make your purchases:
- Online at JHHP.NationsBenefits.com
- Through the Benefits Pro™ App through NationsBenefits®
- At a participating retail location. Use the store locator on the portal or app, or call NationsBenefits.
- By calling 888-959-2069 (TTY: 711) 8 a.m. – 8 p.m. local time
How can I check my Flex Card balance?
You can check your Flex Card balance at JHHP.NationsBenefits.com or through the Benefits Pro™ App. You can also call 888-959-2069 (TTY: 711).
What if there is not enough money in my Flex Card account to cover the entire purchase?
If the purchase amount is more than the available funds on your card, a partial amount will be deducted from the card. You will need to pay the balance with another form of payment.
What if my Flex Card is lost or stolen?
If your Flex Card is lost or stolen you can report it and request a new card in your Benefits Pro™ Portal, Benefits Pro™ App or call NationsBenefits® at 888-959-2069 (TTY: 711).
How do I download the Benefits Pro app?
Open App Store® or Google Play® and search for the Benefits Pro™ App.
Where can I find my member ID number?
It can be found on the front of your health plan ID card.
What is the Over-the-Counter (OTC) benefit?
The benefit lets you get over-the-counter items by going to any allowed stores. You can also order by phone at 1-888-628-2770 (TTY: 711) Monday to Friday, from 9 AM to 8 PM local time or online. You order from a list of approved items, and it will be sent to your address.
How much is my OTC benefit?
The amount depends on your benefit plan. Check your plan documents or call OTC Health Solutions at 888-628-2770 (TTY: 711).
Can I carry over unused benefit amount to the next benefit period?
Unused benefit amounts do not roll over to the next quarter.
Can I order more than my benefit amount?
You cannot exceed your benefit amount online or by phone. However, you may exceed your benefit amount at any allowed CVS Pharmacy® store and pay the difference out of pocket.
Are all items available at the stores?
Not all items are available in stores. Items marked with a truck icon in the catalog can only be ordered over the phone or online.
Can I cancel my order once it has been placed?
Orders can only be canceled within 30 minutes after being placed. To cancel an order, you can use the automated Interactive Voice Response (IVR) system or talk to an agent.
How do I confirm my order was placed?
Once the order is placed, you will receive an order number. Access to order history is also available in the portal/app. Always keep your order number.
Can I track my order?
You can use our automated Interactive Voice Response (IVR) system to track an order. If your phone number or email was added to your account, you will also receive email/ text updates. You can also view tracking information through our Over-the-Counter Health Solutions (OTCHS) portal/app.
How will the items be shipped?
Items are shipped via USPS to your home at no charge to you. Please allow up to 14 days for delivery.
How can I get help if I think I have a problem with opioids?
Call our Behavioral Health Services at 410-424-4476, Monday through Friday from 8 a.m. to 5 p.m.
What else can I do to manage my pain?
- Taking a prescription opioid is not the only option for managing pain successfully. You and your doctor should work together to come up with a pain plan. It may include:
- Understanding how your medications work and how they will impact your body
- Discussing medication risks with your doctor
- Learning about non-opioid options, such as:
- Occupational and/or physical therapy
- Acupuncture
- Chiropractic care
- Stress management or depression treatment
- Over-the-counter remedies, such as ibuprofen
- Ice and heat therapy
- Exercise
- Massage
- Staying active in spite of your pain
- Keeping a pain diary to help guide you and your doctor in managing your pain
- Identifying a support network
- Maintaining a healthy diet
Tips for keeping opioid medications safe
- Put all medication away and out of children’s reach and sight.
- Always relock the cap on the medicine bottle.
- Do not share your medication.
- Safely dispose of unused pills.
What to do with extra medication?
Sharing prescribed medication is illegal and potentially dangerous. If you have extra unused or unwanted medications, please dispose of them through a Drug Take-Back program.
- Johns Hopkins Medicine participates in yearly drug take back events. Check here for more information about upcoming events.
- Search for year-round pharmaceutical disposal locations by zip code.
- While it’s best to use a Drug Take-Back program or location, most opioids are on the FDA Flush List and may be flushed down the toilet to ensure that they are not accidentally or intentionally ingested, touched, misused, or abused.
Why should I be concerned about taking an opioid?
Opioids are highly addictive, even when taken as directed. The longer you take them, the more likely you are to become addicted.
There is also a risk of side effects when taking opioids with certain medications. For example, combining an opioid with a benzodiazepine—like alprazolam (Xanax®), clonazepam (Klonopin®), or diazepam (Valium®)—might cause a dangerous drug interaction that could lead to an accidental overdose.
If you suspect that someone has overdosed, please call 911. You can give the person a medication called Naloxone to reverse the overdose while waiting for a medical response. If you give someone Naloxone, observe them constantly until emergency care arrives to make sure their breathing does not slow or stop. Our formulary includes generic Narcan, a nasal spray containing Naloxone. (You can work with your prescriber or pharmacist to decide the best option for you to have on hand, and check the medication tier by using the formulary search tool.)
Because opioids carry such serious risks, Advantage MD conducts reviews or safety edits whenever a member:
- Receives opioid prescriptions from three or more prescribers and takes a total of 90 Morphine Milligram Equivalents (MME) or more per day,
- Receives prescriptions for both an opioid and a benzodiazepine, OR
- Receives prescriptions for both an opioid and a buprenorphine.
In each of these situations, the pharmacist can override the review or safety edit by consulting with the prescriber(s) to determine the medical necessity of the member’s prescriptions. If the pharmacist is unable or unwilling to override the review or safety edit, the member, member’s representative and/or prescriber can submit a coverage determination.
For members who have not filled an opioid prescription in the past 108 days, we limit their initial opioid prescriptions for treatment of acute pain to no more than a 7-day supply. Pharmacists can override this review by assessing the member’s opioid fill history. The member, member’s representative and/or prescriber can submit a coverage determination to get more than a 7-day supply.
What are some common opioids?
Common prescription opioids include:
- Oxycodone (OxyContin®, Percocet®, Roxicodone®)
- Hydrocodone (Vicodin®, Lorcet®, Norco®)
- Morphine (MS Contin®)
- Codeine (Tylenol® with codeine)
- Tramadol (Ultram®)
- Methadone
How do I safely dispose of medications I don’t need?
The Advantage MD MTM Program is dedicated to providing you with information about safe medication disposal. Medications that are safe for you may not be safe for someone else. Unneeded medications should be disposed of as soon as possible. You can discard your unneeded medications through a local safe disposal program or at home for some medications.
Locating a community safe drug disposal site
A drug take back site is the best way to safely dispose of medications. To find drug take back sites near you, visit the DEA Controlled Substance Public Disposal Locations website and enter your location.
Some pharmacies and police stations offer on-site drop-off boxes, mail-back programs, and other ways for safe disposal. Call your pharmacy or local police department (non-emergency number) for disposal options near you.
Mailing medications to accepting drug disposal sites
Medications may be mailed to authorized sites using approved packages. Information on mail-back sites can be found at www.deatakeback.com.
Safe at-home medication disposal
You can safely dispose of many medications through the trash or by flushing them down the toilet. Learn more about safe at-home disposal.
Follow these steps for medication disposal in the trash:
- Remove medication labels to protect your personal information
- Mix medications with undesirable substances, such as dirt or used coffee grounds
- Place mixture in a sealed container, such as an empty margarine tub
How do I get more information about the Medication Therapy Management Program?
Please contact us if you would like additional information about our MTM program or if you do not want to participate. Call 844-635-3406 (TTY: 711) 24 hours a day, seven days a week.
What is a Targeted Medication Review?
The targeted medication review is completed by a health care provider who reviews your medications at least once every three months. With this review, we mail, fax, or call your prescriber with suggestions about prescription drugs that may be safer or work better for you. As always, your prescriber will decide whether to consider our suggestions. Your prescription drugs will not change unless you and your prescriber decide to change them. We may also contact you by mail or phone with suggestions about your medications.
How do I benefit from talking with a health care provider?
By completing the medication review with a health care provider, you will:
- Understand how to safely take your medications
- Get answers to any questions you may have about your medications or health conditions
- Review ways to help you save money on your drug costs
- Receive a Recommended To-Do List and Medication List to keep and share with your prescribers and/or caregivers
Why is this review important?
Different prescribers may write prescriptions for you without knowing all the medications you take. For that reason, the MTM Program health care provider will:
- Review all your medications
- Discuss how your medications may affect each other
- Identify any side effects from your medications
- Help you reduce your prescription drug costs
Who will contact me about the Medication Therapy Management Program?
You may receive a call from a pharmacy where you recently filled one or more of your prescriptions. You can choose to complete the review in person or over the phone.
A health care provider may also call you to complete your review over the phone. When they call, you can schedule your review at a time that is best for you.
Trusted MTM Program partners: You may receive a call from the CVS Caremark Pharmacist Review Team or the Outcomes Patient Engagement Team to complete this service.
What is a Comprehensive Medication Review?
The comprehensive medication review is completed with a health care provider in person or over the phone. This review is a discussion that includes all your medications:
- Prescription drugs
- Over-the-counter (OTC)
- Herbal therapies
- Dietary supplements
This review usually takes 20 minutes or less to complete. During the review, you may ask any questions about your medications or health conditions. The health care provider may offer ways to help you manage your health and get the most out of your medications. If more information is needed, the health care provider may contact your prescriber.
After your review, you will receive a summary of what was discussed. The summary will include the following:
- Recommended To Do List. Your to-do list may include suggestions for you and your prescriber to discuss during your next visit.
- Medication List. This is a list of all the medications discussed during your review. You can keep this list and share it with your prescribers and/or caregivers.
- Here is a blank copy of the Medication List for tracking your medications
What services are included in the Medication Therapy Management Program?
In the MTM Program, you will receive the following services from a health care provider:
- Comprehensive Medication Review
- Targeted Medication Review
How will I know if I qualify for the Medication Therapy Management Program?
If you qualify, we will mail you a letter. You may also receive a call or text to set up your one-on-one medication review.
Who qualifies for the Medication Therapy Management Program?
You will be enrolled in the Johns Hopkins Advantage MD MTM Program if you meet one of the following:
- Have coverage limitation(s) in place for medication(s) with a high risk for dependence and/or abuse, or
- Meet the following criteria:
- You have three or more of these conditions:
- Alzheimer’s Disease
- Bone disease – arthritis (osteoporosis, osteoarthritis, rheumatoid arthritis)
- Chronic congestive heart failure
- Diabetes
- Dyslipidemia
- End-stage renal disease
- HIV/AIDS
- Hypertension
- Mental health (depression, schizophrenia, bipolar disorder, chronic/disabling mental health conditions)
- Respiratory disease (asthma, COPD, chronic lung disorders)
- You take eight or more routine medications covered by your plan
- You are likely to spend more than $1,623 in Part D prescription drug costs in 2025
- You have three or more of these conditions:
Your participation in the MTM Program is voluntary and does not affect your coverage. This is not a plan benefit and is open only to those who qualify. There is no extra cost to you for the MTM Program.
What is an appointment of representative?
You may name someone to act for you as a representative. This person can be a relative, friend, lawyer, advocate, doctor, or someone else. You may already have someone authorized by the Court or in accordance with State law to act for you. To authorize someone to act as your representative, you and that person must sign and date a statement that gives the person legal permission to do so.
How do I assign an appointment of representative?
To assign an appointment of representative, download, print, and complete the form and mail to either of the following locations.
For coverage determination or appeal-related issues, mail the form to:
Johns Hopkins Advantage MD
c/o CVS/Caremark Part D Services
Coverage Determination & Appeals Dept.
PO BOX 52000 MC 109
Phoenix, AZ 85072-2000
For grievance-related issues, mail the form to:
Johns Hopkins Advantage MD
c/o CVS/Caremark Part D Services
Medicare Part D Grievances Department
P.O. Box 30016
Pittsburgh, PA 15222-0330
For additional information, you may call us 24 hours a day, seven days a week.
PPO members: call 877-293-5325 (TTY: 711).
HMO members: call 877-293-4998 (TTY: 711).
How do I submit an appeal for a denied coverage determination or exception request?
We accept standard and expedited requests by telephone and in writing.
Submit online:
Paper request:
- PPO Paper Prescription Drug Coverage Redetermination Request – English | Spanish
- HMO Paper Prescription Drug Coverage Redetermination Request – English | Spanish
By phone:
You can file a request by phone or call to ask for help submitting your request 24 hours a day, seven days a week.
PPO members: call 877-293-5325 (TTY: 711).
HMO members: call 877-293-4998 (TTY: 711).
Fax:
To fax your written request, use our toll-free fax number: 1-855-633-7673
Mail:
To submit a standard request in writing, mail to:
Johns Hopkins Advantage MD
c/o CVS/Caremark Part D Services
Coverage Determination and Appeals Department
PO BOX 52000 MC 109
Phoenix, AZ 85072-2000
How long before I get an answer to my exception request?
For standard exception requests, we will let you know of our decision within 72 hours after the exception request form is submitted to us with your doctor’s supporting statement.
You also have the option to request an expedited exception request if your doctor believes your health could be seriously harmed by waiting up to 72 hours for a decision. If the coverage determination form submitted to us with your doctor’s supporting statement is considered urgent, and we agree, we will let you know of our decision within 24 hours of your request.
How do I submit exceptions and coverage determination (prior authorization) requests?
Submit online:
Paper request:
- PPO Paper Prescription Drug Coverage Determination Request – English | Spanish
- HMO Paper Prescription Drug Coverage Determination Request – English | Spanish
By phone:
You can file a request by phone or call to ask for help submitting your request 24 hours a day, seven days a week.
PPO members: call 877-293-5325 (TTY: 711).
HMO members: call 877-293-4998 (TTY: 711.
Fax:
To fax your written request, use our toll-free fax number: 1-855-633-7673
Mail:
To submit a standard request in writing, mail to:
Johns Hopkins Advantage MD
c/o CVS/Caremark Part D Services
Coverage Determination and Appeals Department
PO BOX 52000 MC 109
Phoenix, AZ 85072-2000
If we approve your exception request, our approval is typically valid until the end of the plan year as long as your prescribing doctor continues to prescribe the Part D drug for you and it continues to be safe and effective for treating your condition. If we deny your exception request, you may ask for a review of our decision (called a redetermination) by submitting an appeal. You must request this appeal within 60 calendar days from the date of our first decision.
How will I know if a prior authorization, quantity limit or step therapy requirement applies to a drug I take?
To find out if these restrictions apply to a drug you take:
Search for the drug using the online formulary search tool or review your plan’s formulary.
- PPO and Plus (PPO) Formulary Search Tool
- Primary (PPO) Formulary Search Tool
- HMO Formulary Search Tool
- D-SNP (HMO) Formulary Search Tool
- Select (HMO) Formulary Search Tool
- PPO and Plus (PPO) Formulary Formulary – English | Spanish
- HMO Formulary
- Primary (PPO) Formulary
- D-SNP (HMO) Formulary
- Select (HMO) Formulary
Medications that have special requirements for coverage are identified in the formulary with the following indicators:
- PA – Prior Authorization. Our plan requires you or your provider to get prior authorization for certain drugs. This means that you will need to get approval from us before you fill your prescriptions. If you don’t get approval, we may not cover the drug.
- QL – Drug has Quantity limit. For certain drugs, our plan limits the amount of the drug that we will cover. For example, our plan provides 30 tablets per 30 days per prescription for rosuvastatin.
- ST Step Therapy. – In some cases, our plan requires you to first try certain drugs to treat your medical condition, before we will cover another drug for that condition. For example, if Drug A and Drug B both treat your medical condition, we may not cover Drug B unless you try Drug A first. If Drug A does not work for you, we will then cover Drug B.
- NM – Not available at mail order pharmacies.
- B/D – This drug may be covered under Medicare Part B or D depending upon the circumstances; information may need to be submitted describing the use and setting of the drug to make the determination.
- EX – This prescription drug is not normally covered in a Medicare Prescription Drug Plan. The amount you pay when you fill a prescription for this drug does not count towards your total drug costs (that is, the amount you pay does not help you qualify for catastrophic coverage). In addition, if you are receiving extra help to pay for your prescriptions, you will not get any extra help to pay for this drug.
- V/I – This drug’s Tier Copay may not apply to you. Our plan covers most Part D vaccines at no cost to you. Our plan covered insulin is no more than $35 for a one-month supply. Call Customer Service for your estimated cost.
- * – Non-extended day supply. Not available for an extended (long-term) supply
You can also call us toll-free, 24 hours a day, seven days a week.
PPO members: call 877-293-5325 (TTY: 711).
HMO members: call 877-293-4998 (TTY: 711).
What are exceptions?
As a member, you have the right to ask us to make an exception to our plan formulary. Examples of formulary exception requests include asking us to:
- Cover your Part D drug even if it is not included on our formulary. This is referred to as a formulary exception request.
- Provide your drug at a lower copayment if there are drugs for your condition at a lower copayment level. For example, if your drug is included in Tier 2, and there are drugs to treat your condition in Tier 1, you can ask us to cover it at the Tier 1 cost-sharing amount instead. This is referred to as a tiering exception request.
Note: If we grant your request to cover a drug that is not on our formulary, you may not also request a higher level of coverage for the same drug. Also, you may not ask us to provide a higher level of coverage for any Tier 5 (Specialty Tier) drugs.
The best way to request a drug formulary exception, or a tiering exception, is with the help of your prescribing doctor. He or she must provide a written statement that explains the medical reasons for requesting an exception. Your doctor can submit a statement to us using a coverage determination form; however, no specific form is required.
What is a quantity limit?
Certain covered drugs require a quantity limit restriction. That means we will only cover the drug up to a designated quantity or amount. If your prescribing doctor feels it is medically necessary to exceed the set limit, he or she must get prior approval before the higher quantity can be covered. Quantity limits are generally used as a safety precaution to prevent certain prescription drugs from being used excessively. To request a quantity limit exception, you and/or your doctor may complete and submit a coverage determination form. You may download the form and send it back to us or submit your request online through our secure website.
What is a step therapy requirement?
A step therapy requirement means you must first try one drug to treat your medical condition before we will cover another drug for that same condition. For example, if Drug A and Drug B both treat your medical condition, and both are covered drugs, we may require your doctor to prescribe Drug A first. If Drug A does not work for you, then we will cover Drug B. To request a step therapy exception, you and/or your doctor may complete and submit a coverage determination form. You may download the form and send it back to us or submit your request online through our secure website.
- PPO and Plus (PPO) Step Therapy Criteria
- HMO Step Therapy Criteria
- D-SNP (HMO) Step Therapy Criteria
- PPO Paper Prescription Drug Coverage Determination Request – English | Spanish
- HMO Paper Prescription Drug Coverage Determination Request – English | Spanish
- Online Medicare Prescription Drug Coverage Determination
What is a coverage determination (prior authorization)?
For certain prescription drugs, additional coverage or limit requirements may be in place to help our members use these drugs in a safe way, while also helping to control costs for everyone. We, therefore, require you to get a prior authorization (prior approval) before certain drugs will be covered under the plan.
- PPO and Plus (PPO) Prior Authorization Criteria
- HMO Prior Authorization Criteria
- D-SNP (HMO) Prior Authorization Criteria
To request a prior authorization, you and/or your doctor may complete and submit a Coverage Determination form.
Your prescribing doctor will need to tell us the medical reason why your Johns Hopkins Advantage MD plan should authorize coverage of your prescription drug. Without the necessary information on the prior authorization form, we may not approve coverage of the drug.
Submit online:
Paper request:
- PPO Paper Prescription Drug Coverage Determination Request – English | Spanish
- HMO Paper Prescription Drug Coverage Determination Request – English | Spanish
Mail to:
Johns Hopkins Advantage MD
c/o CVS/Caremark Part D Services
Coverage Determination and Appeals Department
PO BOX 52000 MC 109
Phoenix, AZ 85072-2000
When can you end your membership in our plan?
You can only end your membership with Johns Hopkins Advantage MD during certain times of the year. Those include:
- The Annual Enrollment Period (AEP), which happens from October 15 to December 7. If you do so, your membership will end when your new plan’s coverage begins on January 1.
- The Medicare Advantage Open Enrollment period is from January 1 to March 31. During this time you have the opportunity to:
- Switch to a different Medicare Advantage plan
- Return to Original Medicare
If you choose to switch to Original Medicare during this period, you have until March 31 to join a separate Medicare prescription drug plan to add drug coverage. Your membership will end on the first day of the month after we get your request to switch to Original Medicare. If you also choose to enroll in a Medicare prescription drug plan, your membership in the drug plan will begin the first day of the month after the drug plan gets your enrollment request.
- In certain situations, members of Johns Hopkins Advantage MD may be eligible to end their membership at other times of the year if they qualify for a Special Enrollment Period (SEP). To see a full list of examples of situations that meet the criteria for the Special Enrollment period, visit medicare.gov. To find out if you are eligible for a Special Enrollment Period, please call Medicare at 800-MEDICARE (800-633-4227), 24 hours a day, 7 days a week. TTY users call 877-486-2048.
Where can you get more information about when you can end your membership?
If you have questions about ending your membership with Johns Hopkins Advantage MD, please call us.
PPO members: 877-293-5325 (TTY: 711)
HMO members: 877-293-4998 (TTY: 711)
You can also contact Medicare at 800-MEDICARE (800-633-4227), 24 hours a day, seven days a week. TTY users should call 877-486-2048.
You have the right to make a complaint if we end your membership in our plan
If we end your membership in our plan, we will tell you our reasons in writing for ending your membership and tell you how you can make a complaint about our decision to end your membership.
What is a quality of care complaint?
A Quality of Care Complaint may be filed through the standard grievance process outline above. A quality of care complaint can also be filed with the Quality Improvement Organization (QIO) in Maryland. The QIO is a group of practicing doctors and other health care experts paid by the Federal government to check and improve the care given to Medicare patients. If you wish, you can complain to us and the QIO at the same time.
To contact the QIO:
Call: 888-396-4646 (TTY 888-985-2660)
Write:
Livanta BFCC-QIO Program 10820 Guilford Road, Suite 202 Annapolis Junction, MD 20701
What is a grievance resolution?
After you file your complaint, we will investigate it. For all grievances, you will receive a written notice stating the results of the review. We must address your grievance as quickly as your case requires based on your health status, but no later than 30 days after receiving your grievance. We must respond whether we agree with your complaint or not. We may extend the time frame by up to 14 days if you ask for an extension, or if we identify a need for additional information and the delay is in your best interest. Most complaints are answered within 30 days.
What is an expedited (fast) grievance?
You also have the right to ask for an expedited (fast) grievance. Any fast grievance must be resolved within 24 hours from the time you contact us. You have the right to request a fast grievance if you disagree with:
- The 14-day extension on “fast coverage decision” or “fast appeal”; or
- Our denial of your request to expedite a coverage decision or reconsideration for health services.
Upon receipt of the grievance, we will promptly investigate the issue you have identified. If we agree with your grievance, then we will cancel the 14-day extension and expedite the determination or appeal as you originally requested. Regardless of whether we agree or not, we will notify you of our decision by phone within 24 hours and will send you written follow up.
If you are making a complaint because we denied your request for a “fast coverage decision” or a “fast appeal” we will automatically give you a “fast” complaint. If you have a “fast complaint” it means we will give you an answer within 24 hours.
How do I file a grievance?
You can file a grievance with us by mail, fax, or telephone.
Call:
We are available October 1 through March 31, Monday through Sunday 8 a.m. to 8 p.m., and April 1 through September 30, Monday through Friday 8 a.m. to 8 p.m.
PPO members: 877-293-5325 (TTY: 711)
HMO members: 877-293-4998 (TTY: 711)
If there is anything else you need to do, we will let you know.
If you do not wish to call (or you called and were not satisfied), you can put your complaint in writing and mail it to us.
Write:
Johns Hopkins Advantage MD Appeals and Grievances, P.O. Box 3507, Scranton, PA 18505
Fax:
855-825-7726
Who may file a grievance?
You or your appointed legal representative may file a grievance. You may name a relative, friend, attorney, doctor or someone else to act for you. Others may already be authorized under state law to act for you. You may download the appointment of representative form.
Contact us promptly either by phone or in writing. Your complaint must be filed within 60 days of the event or incident.
What is a grievance?
The formal name for “making a complaint” is “filing a grievance.” A grievance is a type of complaint you make about the health plan or one of our network providers, including a complaint concerning the quality of your care. This type of complaint does not involve coverage or payment disputes.
What are the deadlines for a “fast” appeal?
When we are using the fast deadlines, we must give you our answer within 72 hours after we receive your appeal. We will give you our answer sooner if your health requires us to do so. However, if you ask for more time, or if we need to gather more information that may benefit you, we can take up to 14 more calendar days. If we decide to take extra days to make the decision, we will tell you in writing.
If we do not give you an answer within 72 hours (or by the end of the extended time period if we took extra days), we are required to automatically send your request on to Level 2 of the appeals process, where it will be reviewed by an independent organization.
What are the deadlines for a “standard” appeal?
If we are using standard deadlines, we must give you our answer within 30 calendar days after we receive your appeal if your appeal is about coverage for services you have not yet received. For post service appeals (appeals about coverage have already received), we must give you our answer within 60 calendar days after we receive your appeal. We will give you our decision sooner if your health condition requires us to.
However, if you ask for more time, or we need to gather more information that may benefit you, we can take up to 14 more calendar days. If we decide to take extra days to make the decision, we will tell you in writing.
If we do not give you an answer by the deadline above (or by the end of the extended time period if we took extra days), we are required to send your request on to Level 2 of the appeals process, where it will be reviewed by an independent outside organization.
What happens when I make an appeal?
When you appeal a decision for the first time, this is called a Level 1 Appeal. In this appeal, we review the coverage decision we made to check to see if we were following all of the rules properly. Your appeal is handled by different reviewers than those who made the original unfavorable decision. When we have completed the review, we give you our decision. Under certain circumstances, which we discuss later, you can request an expedited or “fast coverage decision” or fast appeal of a coverage decision.
If we say no to all or part of your Level 1 Appeal, you can go on to a Level 2 Appeal. The Level 2 Appeal is conducted by an independent organization that is not connected to us. (In some situations, your case will be automatically sent to the independent organization for a Level 2 Appeal. If this happens, we will let you know. In other situations, you will need to ask for a Level 2 Appeal). If you are not satisfied with the decision at the Level 2 Appeal, you may be able to continue through additional levels of appeal.
How do I make an appeal?
You must make your appeal request within 60 calendar days from the date on the written notice we sent to tell you our answer to your request for coverage decision. For specific instructions on how to file an appeal, you or your representative may:
Call:
PPO members: 877-293-5325 (TTY: 711)
HMO members: 877-293-4998 (TTY: 711)
Write:
NEW: Johns Hopkins Advantage MD Appeals, P.O. Box 8777, Elkridge, MD 21075
Fax:
NEW: 410-424-2806
All appeals requests must include a completed and signed Waiver of Liability Form.
If you have questions about the appeals process or would like to know the status of an appeal you’ve filed, please call us. We are available October 1 through March 31, Monday through Sunday 8 a.m. to 8 p.m., and April 1 through September 30, Monday through Friday, 8 a.m. to 8 p.m.
What is an appeal?
If we make a coverage decision that you are not satisfied with, you can “appeal” the decision. An appeal is a formal way of asking us to review and change a decision we have made.
How do I request an expedited or fast coverage decision?
Under certain circumstances you can request an expedited coverage decision which is also called a “fast track appeal.” A fast track appeal means that we will make a decision no later than 72 hours after receiving the request.
To get a fast track appeal you must meet both of the following requirements:
- You are asking for coverage for medical care you have not yet received
- Using the standard deadlines could cause serious harm to your health or hurt your ability to function. If we determine that your request does not meet the criteria above, then it will be handled as a standard coverage decision
If we process your request as a fast track appeal we may need extra time to gather information. If we decide to take extra days, we will tell you in writing. If you believe we should not take extra days, you can file an expedited or “fast grievance” also known as a “fast complaint.” See the grievance process below for more information about the grievance process.
How do I request a coverage decision?
As a member of Advantage MD, you have a right to request a coverage decision. If the plan denies coverage for your requested item or service, you have the right to appeal and ask us to reconsider the decision. You also have a right to file a grievance (also called a complaint) about the health plan.
To request a coverage decision regarding medical care you or your representative may:
Call:
We are available October 1 through March 31, Monday through Sunday 8 a.m. to 8 p.m., and April 1 through September 30, Monday through Friday 8 a.m. to 8 p.m.
PPO members: 877-293-5325 (TTY: 711)
HMO members: 877-293-4998 (TTY: 711)
Fax:
855-206-9203
Write:
Johns Hopkins Advantage MD, PO BOX 3538, Scranton, PA 18505
To request a coverage decision regarding payment requests you or your representative may:
Call:
We are available October 1 through March 31, Monday through Sunday 8 a.m. to 8 p.m., and April 1 through September 30, Monday through Friday 8 a.m. to 8 p.m.
PPO members: 877-293-5325 (TTY: 711)
HMO members: 877-293-4998 (TTY: 711)
Fax:
855-206-9203
Write:
Johns Hopkins Advantage MD, PO BOX 3537, Scranton, PA 18505
What is a coverage decision?
A coverage decision is any decision made by the plan regarding:
- Receipt of, or payment for, a care item or service
- The amount you pay for an item or service
- A limit on the quantity of items or services
Any time that we make a decision about what we will cover and how much we will pay for your medical services or drugs, we are making a coverage decision.
Where do I get more information about Advantage MD’s appeals, grievance, and coverage decision process?
Chapter 9 of your plan’s EOC will provide more specific information about our process for appeals, grievances, and coverage decisions. You may also give us a call with questions or concerns or to obtain an aggregate number of grievances, appeals, and exceptions. We are available October 1 through March 31, Monday through Sunday 8 a.m. to 8 p.m., and April 1 through September 30, Monday through Friday 8 a.m. to 8 p.m.
PPO members: 877-293-5325 (TTY: 711)
HMO members: 877-293-4998 (TTY: 711)
What if my authorization is not approved?
You should share a copy of the decision with your doctor so you and your doctor can discuss next steps. If we make a coverage decision and you are not satisfied with this decision, you or your provider can “appeal” the decision. An appeal is a formal way of asking us to review and change a coverage decision we have made. The directions on how to file an appeal are in your notification letter or in Chapter 9 of your Evidence of Coverage.
What do I do if my treatment requires prior authorization or step therapy?
Your provider is responsible for submitting the prior authorization or step therapy exception request. Your provider is aware of how to submit this request. Once Advantage MD reviews the request, you will be notified of the decision via phone and mail. Please contact your provider to determine next steps.
How do I determine if my treatment requires prior authorization or step therapy?
All preferred and non-preferred Part B drugs are identified on the Advantage MD Part B Prior Authorization List. Look for your drug on the list. If your drug is not listed, it does not require prior authorization. If it is listed as a Preferred Product, it does not require step therapy.
How do I get reimbursed for vaccines?
Sometimes when you get a vaccine and/or the shot at a non-network pharmacy or at the physician’s office, you may need to pay the full cost right away. Other times, you may find that you have paid more than expected under the coverage rules of the plan. In either case, you can ask our plan to pay you back (reimburse).
To speed up the reimbursement process and to make sure that you are giving us all the information we need, you should complete the Medicare Part D Prescription Claim Form and send this form along with a detailed receipt for the vaccine and the pharmacy label, or your pharmacy prescription claim history to us. (The pharmacy label is generally attached to your prescription bag when you pick up your medication and includes the name of the drug, quantity, date of purchase, and cost of the drug. Your pharmacy prescription claim history is a print out of what prescription you filled and paid for.)
You do not have to use the Medicare Part D Prescription claim form, but the use of this form will speed up the reimbursement process.
Medicare Part D Prescription Claim Form
Please mail your request for payment together with any receipts to:
Johns Hopkins Advantage MD
c/o CVS/caremark Part D Services
PO BOX 52066
Phoenix, AZ 85072-2066
If you have any questions, you can call Customer Service 24 hours a day, seven days a week.
PPO members: call 877-293-5325 (TTY: 711).
HMO members: call 877-293-4998 (TTY: 711).
See Chapter 7 of your Evidence of Coverage for additional information on the reimbursement process.
Please note: the information in this section does not apply to Advantage MD Group.
How do I know which vaccines are covered by Part D?
Part D vaccines are listed in your plan’s formulary.
- PPO and Plus (PPO) formulary – English | Spanish
- Primary (PPO) formulary
- HMO formulary
- Select (HMO) formulary
- D-SNP (HMO) formulary
Are all vaccines covered under Part D?
No, the following vaccines and their administrations are covered under your Advantage MD Part B medical benefit:
- Influenza
- Pneumococcal
- COVID-19
Part B vaccines are available from your provider’s office or a network pharmacy. Show the pharmacist your Advantage MD member ID card to receive these vaccinations at no cost to you.
What is HealthLINK@Hopkins?
HealthLINK@Hopkins is your personal member portal. It is a secure, online hub for Johns Hopkins Advantage MD (HMO/PPO) members and their in-network providers.
What should I use my member portal for?
We encourage you to sign into your member portal often, especially after you seek health care. You can keep and monitor a personal record of your health care visits and services.
You can also use your portal to:
- Check the status of claims and referrals
- Search for a provider
- Review your benefits
- Print a temporary member ID card
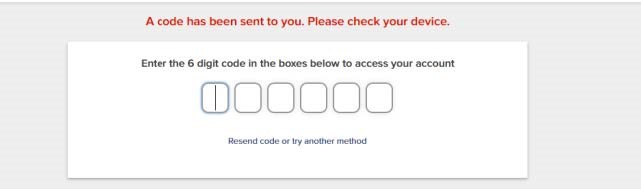
How do I set up 2 factor authentication?
When you try to log into HealthLINK, after entering your user name and password, you will be brought to this page:
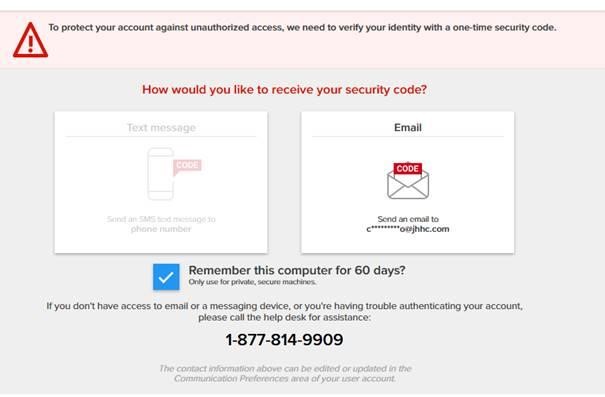
You will be prompted to receive a security code either through text, (if you have a cell phone number listed in your account) or by email. If you don’t have any cell phone listed in your account, you can add it later by scrolling down to the “Communication Preference” section of the Administration tab. (See the NOTE for instructions). If you request the code through email, and it does not appear in your inbox, check your spam/junk folder.
NOTE: Changing Communication Preferences After completing the two-factor authentication process using your email and successfully entering the HealthLINK portal, go to the Administration tab and scroll down to Communication Preferences.
Go to “Edit Contact Details”
Enter your mobile number and choose “Save.”
How do I register for an account?
- Go to HealthLINK@Hopkins.
- Select “Member Register” under “First Time Logging In?” on the right side of the page.
- Follow the instructional screens to register and create a user ID and password.
- Your password must be at least nine characters and must contain at least one uppercase letter, one lowercase letter, one number, and one special character, such as #, *, or @
- Usernames and passwords are case-sensitive.
Remember: your password is private so don’t write it down or keep it in a public space. Once the process is complete, you will be able to access your account.
What happens if I can’t remember my password?
When registering for a HealthLINK@Hopkins account, you will be asked to choose 3 security questions and provide answers. In the event that you ever forget your password, you can change it by correctly answering your security questions.
If you still can’t remember your password, you will have to call Customer Service directly at 877-814-9909 Member option #2. For security purposes, Johns Hopkins Advantage MD outsources this Customer Service function to another company, HealthTrio.
HealthTrio’s Customer Service will ask you your security question. If you do not answer correctly, you will be locked out of your account until we are notified and can verify your membership. You will be contacted upon verification and you will be able to reset your password and access your HealthLINK@Hopkins account.
Now that I’m logged in, how do I get started?
Once you’re logged in, you’ll see a welcome message on your homepage. This will change periodically to keep you up-to-date and informed on health issues.
Start browsing the site by using the links located in the top navigation bar. They are organized by different sections including My Providers, My Health Plan, My Resources and My Preferences.
You will also find a list of Quick Links in the left column of tasks most used by Advantage MD members.
How do I search for a provider?
Choose “Provider Search”, under the tab “My Health Plan” in the top navigation bar. You can also choose “Search for a Provider” in the left column under Quick Links on the home page.
Why aren’t there any results when I search for a provider?
First, make sure you are spelling the provider’s name correctly. If you aren’t sure of the spelling, type in the first three letters and a list will generate all doctors with a last name starting with those letters. You can then browse the list manually. Your search may also be too narrow, meaning there are no providers with your selected criteria within your network. Broaden your search by typing %% in a field or leaving it blank. This will generate all providers within those fields. Lastly, your search may also be too broad, in that there are far too many providers with your criteria for a list to generate. You can narrow your search by selecting an option in a field. A list will generate only those doctors that fit your criteria.
What is “View Audit”?
This button allows you to see all of your account transactions. If you’d like further information about any of the transactions, write down the complete transaction ID and contact customer service.
PPO members: 877-293-5325 (TTY: 711)
HMO members: 877-293-4998 (TTY: 711)
Why aren’t my claims appearing?
Claims status will be updated to HealthLINK in 2-5 business days after your claim has been processed. Most claims are processed within 30 days after receipt. If you’d like to confirm receipt or check the status of a claim, you can also call Customer Service.
PPO members: 877-293-5325 (TTY: 711)
HMO members: 877-293-4998 (TTY: 711)
How can I receive a replacement member ID card?
To replace your card, contact Customer Service toll-free at 1-877-293-5325 (TTY: 711). Operating hours are 8 a.m. – 8 p.m., 7 days a week. From February 15 – September 30, you will need to leave a message on weekends and holidays.
You can print a temporary member ID card by logging into HealthLINK. Under My Health Plan, click Member Information then click on Print ID Card.
How do I get reimbursed from the plan if I pay at an out-of-network pharmacy?
If you must use an out-of-network pharmacy, you will generally have to pay the full cost (rather than your normal share of the cost) at the time you fill your prescription. You can ask us to reimburse you for our share of the cost.
Send us your request for payment, along with your bill and documentation of any payment you have made. It’s a good idea to make a copy of your bill and receipts for your records.
To make sure you are giving us all the information we need to make a decision, you can fill out our claim form to make your request for payment.
You don’t have to use the form, but it will help us process the information faster.
Mail your request for payment together with any bills or receipts to us at this address:
Johns Hopkins Advantage MD
c/o CVS/caremark Part D Services
PO BOX 52066
Phoenix, AZ 85072-2066
If you don’t know what you should have paid, or if you received bills and you don’t know what to do about those bills, we can help. If you have any questions, you can contact us 24 hours a day, seven days a week.
PPO members: call 877-293-5325 (TTY: 711).
HMO members: call 877-293-4998 (TTY: 711).
When can I use a pharmacy that is not in the plan’s network?
Generally, Johns Hopkins Advantage MD covers drugs filled at out-of-network pharmacies only when you are not able to use a network pharmacy.
Here are the circumstances when we would cover prescriptions filled at an out-of-network pharmacy:
- The prescription is for a medical emergency or urgent care.
- You are unable to get a covered drug in a time of need because there are no 24-hour network pharmacies within a reasonable driving distance.
- The prescription is for a drug that is out-of-stock at an accessible network retail or mail service pharmacy (including high-cost and unique drugs).
- If you are evacuated or otherwise displaced from your home because of a Federal disaster or other public health emergency declaration.
- A vaccine or drug administered in your doctor’s office.
If you are experiencing any of these situations, you can call us 24 hours a day, seven days a week so we can see if there is a network pharmacy nearby.
PPO members: call 877-293-5325 (TTY: 711).
HMO members: call 877-293-4998 (TTY: 711).
Note: It may cost you more to obtain your medications at an out-of-network pharmacy. If you do need to go to an out-of-network pharmacy for any of the reasons listed above, the plan will cover up to a one-month supply of drugs.
I am moving, but staying within the Johns Hopkins Advantage MD service area, and I plan to continue my enrollment in the plan. What do I need to do to update my address?
You must contact Social Security Administration at 800-772-1213, Monday through Friday, 8 a.m. – 5:30 p.m. In addition, you must contact Johns Hopkins Advantage MD Customer Service at 877-293-4998 (HMO) or 877-293-5325 (PPO). From October 1 – March 31, our Customer Service hours are Monday through Sunday 8 a.m. – 8 p.m. From April 1 – September 30, our hours are Monday through Friday 8 a.m. – 8 p.m.
I am thinking about enrolling in the Johns Hopkins Medicare Advantage plan. How do I know if I am eligible to join?
To join, you must be entitled to Medicare Part A, be enrolled in Medicare Part B, and live in the plan’s service area.
The Johns Hopkins Advantage MD (HMO), Johns Hopkins Advantage MD D-SNP (HMO), and Johns Hopkins Advantage MD (PPO) service area includes the following counties in Maryland: Anne Arundel, Baltimore, Carroll, Frederick, Howard, Montgomery, Somerset, Washington, Wicomico, and Worcester. The Johns Hopkins Advantage MD Plus (PPO) service area include the following counties in Maryland: Anne Arundel, Baltimore, Carroll, Frederick, Howard, Somerset, Washington, Wicomico, and Worcester. The Johns Hopkins Advantage MD Premier (PPO) service area includes Montgomery County only. The Johns Hopkins Advantage MD Tribute (HMO) and Johns Hopkins Advantage MD Primary (PPO) service area includes the following counties in Maryland: Anne Arundel, Baltimore, Frederick, Howard, and Montgomery The Johns Hopkins Advantage MD Select (HMO) service area includes the following counties in Virginia: Arlington, Fairfax City, and Falls Church City.
My income is limited. Is there help available?
If you meet certain income and resource limits, you may qualify for Extra Help from Medicare to pay the costs of Medicare prescription drug coverage. Visit the Social Security Administration’s website (www.ssa.gov) to see if you qualify. Maryland residents may also be eligible for the Senior Prescription Drug Assistance Program (SPDAP). For more information, visit www.marylandspdap.com.
Can I assume that a provider is in-network based on their location or hospital affiliation?
No, it is always best to verify the network status of your specific provider. Providers may have permission to practice at a facility, but may not be contracted with Advantage MD, which can impact the use of your benefits and your out-of-pocket costs. To check our Provider Directory, please visit www.hopkinsmedicare.com/find-a-provider.
Do I need to verify if my provider is in-network before having services performed?
Advantage MD recommends verifying your provider’s network status regularly and especially before receiving services. It is important to verify because providers can opt out of the plan at any time throughout the year. To check our Provider Directory, please visit www.hopkinsmedicare.com/find-a-provider.
How do I find out more information about medication prior authorization?
Some medications require prior authorization from your plan before they can be dispensed by your in-network pharmacy. This helps us ensure that your prescriptions are medically necessary. To determine if a medication requires prior authorization, refer to the Pharmacy Formulary specific to your Advantage MD plan. Your physician can request these medications by submitting a prior authorization request. Information about covered medications, medication prior authorization requirements and pharmacy plan benefits are available here.
What is a Site of Service?
Site of service is a term used to indicate the facility in which you receive care. Many surgical procedures can be performed safely in an outpatient hospital setting, such as an ambulatory surgery center (ASC). Certain procedures require prior authorization when performed in an outpatient hospital setting. For information on covered outpatient services specific to your Advantage MD plan, refer to your Advantage MD Evidence of Coverage.
Does your HMO plan require referrals to see a specialist?
Yes, our HMO plan requires referrals for specialist visits. Your PCP will help coordinate your care with any specialists you may require. Johns Hopkins Advantage MD is a Medicare Advantage Plan with a Medicare contract offering HMO and PPO products. Enrollment in Johns Hopkins Advantage MD HMO or PPO depends on contract renewal.
What is a Referral?
A referral is a written order from your PCP giving you permission to see a specialist or receive certain medical services. For Advantage MD HMO and D-SNP plans, you will need a referral from your PCP before you can see a specialist and be covered for that care. For information on getting a referral for care specific to your Advantage MD plan, refer to your Advantage MD Evidence of Coverage.
What is Prior Authorization?
Certain medical services and supplies may require approval before they will be covered by your plan, such as specialty medical care, inpatient mental health treatment or inpatient substance-abuse treatment.
Your Evidence of Coverage indicates which services, supplies or medications require prior authorization. For Advantage MD PPO, Plus PPO and Premier PPO plans, no prior authorization is required for out-of-network providers eligible to participate in Medicare and most services and supplies as long as the services are covered benefits and medically necessary. All prior authorization requests are coordinated through your primary care physician (PCP), so your provider must ask for and receive approval before you receive care. Johns Hopkins Advantage MD will review the service, drug or equipment to determine the necessity or appropriateness of the services being authorized. If prior authorization is not given, then coverage for care, services or supplies may be limited or denied.
For more information on prior authorization guidelines specific to your Advantage MD plan, refer to your Advantage MD Evidence of Coverage.
What happens if I go to an out-of-network provider in your HMO plan?
If you use providers that are not in our network, the plan may not pay for these services. For more information, review your Evidence of Coverage.
What is the difference between an HMO and a PPO?
Advantage MD offers both HMO and PPO products. With an HMO plan, you must select a primary care provider (PCP) from our network who will coordinate your care. Your PCP will refer you to specialists or hospitals if you require additional care. You must get your care from providers that are in the Advantage MD network; if you go to a provider outside of our network for non-emergency care, you will be responsible for the entire cost.
With a PPO plan, you have the freedom to choose physicians and specialists from within our network, or seek care out of network. If you choose to see a provider that is not in the Advantage MD network, your out-of-pocket costs will be higher.
What is a late enrollment penalty?
An LEP is an additional charge for not previously being enrolled in a Part D Plan. The late enrollment penalty is not determined by the Johns Hopkins Advantage MD plan. This penalty is determined by Medicare for the number of months not enrolled in a Part D Plan, if for any continuous period of 63 days or more after your Initial Enrollment Period is over, you go without one of these:
- A Medicare Prescription Drug Plan (Part D)
- A Medicare Advantage Plan (Part C) (like an HMO or PPO)
- Another Medicare health plan that offers Medicare prescription drug coverage
- Creditable prescription drug coverage.
What if my premium is not paid on time?
Failure to pay your Advantage MD premium will result in being dis-enrolled from the plan. The plan encourages all members to make timely payments, by the first of every month. If a payment is not received for 3 consecutive months you will be dis-enrolled from the plan.
How can I pay my Advantage MD premium?
You can pay your premium by using electronic funds transfer (EFT) from your bank account or have it automatically deducted from your Social Security or Railroad Retirement Board (RRB) benefit check. Y ou can also receive a monthly statement.
The Social Security/RRB deduction may take two or more months to begin after Social Security or RRB approves the deduction. In most cases, if Social Security or RRB accepts your request for automatic deduction, the first deduction from your Social Security or RRB benefit check will include all premiums due from your enrollment effective date up to the point withholding begins. If Social Security or RRB does not approve your request for automatic deduction, we will send you a paper bill for your monthly premiums. You must pay your premium directly to Advantage MD.
Will the amount I pay each month for Advantage MD (insurance premium) change throughout the year?
Your premium will stay the same every month during the calendar year unless you receive a Part D Late Enrollment Penalty (LEP) from the Social Security Administration.
What is Medicare Part D?
Part D: Standalone Prescription Drug Plans
Helps cover some of your prescription drug costs. These plans are offered by private insurance companies who are contracted by Medicare — when you have Part D, you pay a second monthly premium in addition to Medicare. To enroll, you must be enrolled in Original Medicare and live within the plan’s service area. A late enrollment penalty may apply if you choose to enroll after your Initial Enrollment Period.
What is Medicare Part C?
Part C: Medicare Advantage Plans
A Medicare Advantage plan is not the same thing as a Medicare Supplement plan. Advantage plans cover everything that Medicare Part A and Part B do, as well as the expenses that Part A and Part B don’t. Medicare Advantage plans often include extra benefits. For example, Advantage MD includes prescription drugs, vision, hearing, dental and fitness programs. These plans are offered by private insurance companies contracted by Medicare. To enroll, you must have Original Medicare (Parts A and B) and live within the plan’s service area.
What is Medicare Part B?
Part B: Physician & Outpatient Services
Helps cover doctor visits, lab tests, outpatient services and outpatient surgery, and some medical supplies. Eligibility is the same as Part A. Medicare charges a monthly premium for Part B that you must continue to pay, and you will have deductibles and coinsurance costs to cover. A late enrollment penalty may apply if you choose to enroll after your Initial Enrollment Period.
What is Medicare Part A?
Part A: Hospital Services
Helps cover inpatient hospital and nursing home care, home health care, skilled nursing facility care and hospice. You must be at least age 65, a U.S. citizen or permanent resident and you or your spouse must have paid into Social Security for at least 10 years. While Part A is free for most, you will have deductibles and coinsurance costs to cover.
What Can I Expect After Enrolling?
After your enrollment is complete, you’ll receive a member welcome kit within 10 days. Your membership ID card will also be mailed to you. Once you’re a member, you can begin to explore all of the advantages of Advantage MD.
Medicare beneficiaries may also enroll in Johns Hopkins Advantage MD through the CMS Medicare Online Enrollment Center located at www.medicare.gov.
Are There Other Times I Can Enroll?
If you’ve been eligible for Medicare for a while, your enrollment options may be different depending on the time of the year.
Annual Enrollment Period (AEP) (From October 15 – December 7).
AEP takes place at the same time each year. During this period, you can enroll, disenroll — or change your Medicare plans (Medicare Advantage, Medicare Supplement, or prescription drug plan). You also have the option to return to Original Medicare. Elections made during AEP are effective on January 1 of the following year.
“Lock-in Period” (From April 1 – October 14)
Between April 1 and October 14 you cannot change coverage, unless you qualify for a Special Enrollment Period (SEP). If you do not qualify for an SEP, you’ll have to wait until AEP to elect new coverage.
Special Enrollment Period (SEP) (Timing is dependent)
During an SEP, you can enroll, disenroll or change your coverage because of personal circumstances. Reasons for qualifying for SEP may include: you’ve moved, you became eligible for Medicare and Medicaid, you’re leaving your employer group health plan.
Enrolling After 65?
Learn what your options are.
When Can I Enroll?
You can enroll in Medicare as early as three months before your 65th birthday, and up to three months after. This Initial Enrollment Period gives you a 7-month window to sign up.
Keep in mind, you don’t have to be retired to sign up. If you’re one of the millions of people working past 65, you can still enroll. Be sure to check with your benefits department to see if you could save money on your health benefits by enrolling in Medicare.
Am I Eligible For Advantage MD?
To be eligible for a Medicare Advantage plan, you must fall under the following criteria:
- You’re entitled to Part A and enrolled in Part B
- Includes people under 65 years of age who are entitled to Social Security disability.
- You permanently live in the plan’s service area
See a list of eligible counties.
What are the Part D stages?
For 2025, there are three drug stages to Part D coverage: Deductible stage, Initial Coverage stage and Catastrophic Coverage stage.
What is the Deductible stage?
The Deductible Stage is the first payment stage for your drug coverage. The deductible doesn’t apply to covered insulin products and most adult Part D vaccines, including shingles, tetanus, and travel vaccines. You will pay a yearly deductible of $590 on Tier 3, Tier 4 and Tier 5 drugs. You must pay the full cost of your Tier 3, Tier 4 and Tier 5 drugs until you reach the plan’s deductible amount. For all other drugs, you will not have to pay any deductible. The full cost is usually lower than the normal full price of the drug since our plan has negotiated lower costs for most drugs at network pharmacies. Once you have paid $590 for your Tier 3, Tier 4 and Tier 5 drugs, you leave the Deductible stage and move on to the Initial Coverage Stage.
What is the Initial Coverage stage?
During the Initial Coverage stage, Advantage MD shares the cost of your covered prescription drugs, and you pay your share (your copay or co-insurance amount). You pay a copay for drugs in Tiers 1 and 2 and a co-insurance for drugs in Tiers 3, 4 and 5. You are in the Initial Coverage stage until your out-out-pocket costs total $2,000 — this is the maximum you will spend on covered drugs in 2025. You then move on to the Catastrophic Coverage stage.
What is the Catastrophic Coverage stage?
After you reach the out-of-pocket maximum of $2,000 for 2025, you enter the Catastrophic Coverage stage. Once you are in the Catastrophic Coverage stage, you will stay in this payment stage until the end of the calendar year. During this payment stage, you pay nothing for your covered Part D drugs and for excluded drugs* that are covered under our enhanced benefit.
*Advantage MD D-SNP (HMO) does not have excluded drug coverage.
If I enroll in a Medicare Advantage plan, will I lose my Original Medicare?
No. You will not lose Original Medicare coverage if you enroll in our plan. You’re just choosing to allow a private company to administer your benefits instead of the federal government. You do not lose your Medicare benefits and you must continue to pay your Part B premium.
Are the Advantage MD plans Medicare Supplement plans (F+G)?
No. Johns Hopkins Advantage MD (HMO, HMO D-SNP, PPO, PPO Plus, PPO Primary, and PPO Premier) are Medicare Advantage Prescription Drug plans, also known as Medicare Part C. Our contract with CMS allows us to provide you with all the benefits of Original Medicare, plus coverage to help pay for benefits and services that Medicare doesn’t cover. All Advantage MD plans include prescription drug benefits and extras like vision, hearing, dental, and health and wellness programs. (except HMO Tribute which does not include prescription drug benefits).
Still have questions?
Our Customer Service team is here to assist. Contact us via phone or email with any questions you have.

